Post-operative pancreatitis is not universally accepted as a legitimate clinical entity, and the condition is not even precisely defined. But new findings from case series and literature reviews seem to confirm the relevance and importance of the diagnosis, according to presentations at DDW® 2021 that debated the validity of post-pancreatectomy acute pancreatitis.
“It’s a novel topic, a very hot topic, in the field of pancreatic surgery. The concept of pancreatitis happening after an operation is in and of itself not new, but it’s gaining a lot more traction, especially in the past few years,” said presenter Nicholas J. Zyromski, MD, of Indiana University School of Medicine, who argued the “con” side of the debate. “The frequency of its occurrence and the true definition is definitely not clear. So then, what do we do with that once we recognize the problem? That’s obviously the next question.”
His colleague arguing the “pro” side, Giovanni Marchegiani, MD, PhD, of Verona University Hospital in Italy, acknowledged that many audience members likely remain unconvinced that the diagnosis is valid.
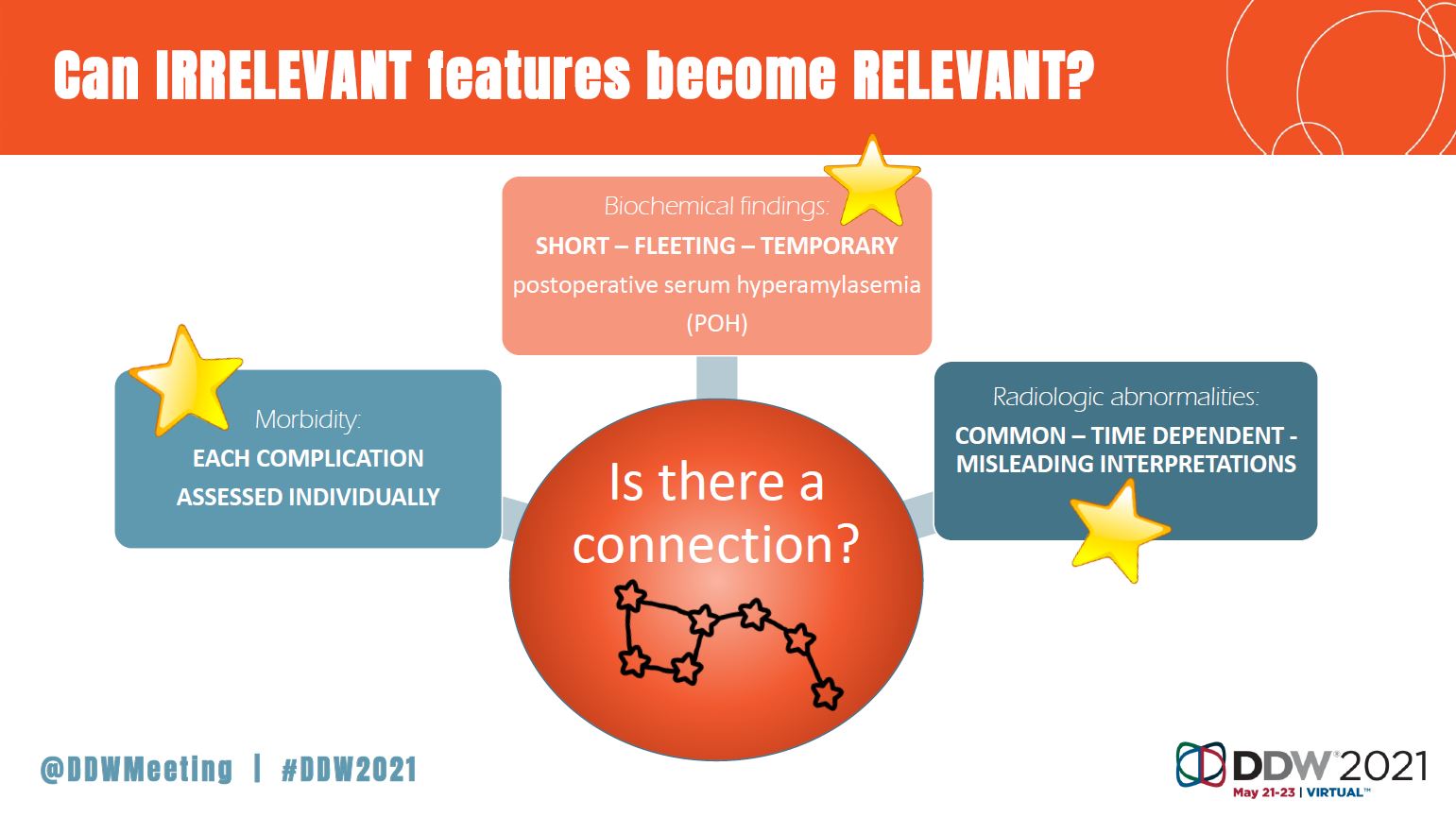
To counter that perception, Dr. Marchegiani described multiple case studies of post-operative clinical complications, including grade C pancreatic fistula; biochemical leak and grade B post-pancreatectomy hemorrhage; and grade B delayed gastric emptying. Certain commonalities seem to underlie these various problems, he said, including:

- Biochemical findings, specifically an increase in serum amylase.
- Radiologic abnormalities, which can often be misinterpreted.
- The presence of a wide range of comorbidities — such as fistulas and abscesses — that are unique to each patient.
- A clinical prognosis that also can vary by individual and can include, in some cases, an increased risk of mortality.
“Can we speculate that there might be a common origin at the beginning of this complicated clinical course? In other words, as in the field of astronomy, can we hypothesize that there could be a single process at the beginning of everything that could explain at least the majority of the complicated clinical scenarios,” asked Dr. Marchegiani. “Keeping all of these factors together, they might look to us like a constellation, and the answer is ‘yes.’”
Despite being tasked with opposite sides of the argument, the debaters ended up agreeing that post-pancreatectomy acute pancreatitis is, indeed, real, but that it needs to be further researched to clarify mechanisms of action, as well as mitigation and intervention strategies.
“This entity exists, the definition is emerging and further research should be directed to understanding the pathophysiology,” said Dr. Zyromski. “And the most important question is: can we standardize a peri-operative management protocol?”
“Maybe I did not convince [audiences] that post-pancreatectomy acute pancreatitis is a clinically relevant condition,” said Dr. Marchegiani, “But at least, I hope that they will now look at the same sky with a different set of eyes.”
Dr. Zyromski’s and Dr. Marchegiani’s oral presentations in “SSAT GI Surgery Debate: Hepatobiliary & Pancreas: Post-Pancreatectomy Acute Pancreatitis is a Relevant Clinical Entity” took place on Sunday, May 23, at 10:45 a.m. EDT.