Ablating the cells that produce the hunger hormone ghrelin leads to weight loss and increased satiety according to a new study by Christopher McGowan, MD, founder and CEO of True You Weight Loss, who is presenting the results during Digestive Disease Week® (DDW) 2024.
“We’ve learned that ablating the lining of the stomach not only destroys hunger-producing cells, but also tightens and shrinks that area,” says Dr. McGowan. “This leads to a reduction in capacity and meaningful weight loss.”

“We need as many treatment options as possible to address the burden of obesity,” says Dr. McGowan. “GLP-1 agonists have gained a lot of popularity recently, but we know that they are not the answer for every person with obesity. Some patients find a one-time procedural intervention more attractive than long-term medications.”
In this first-in-human study, Dr. McGowan treated 10 adult patients with obesity via endoscopic gastric fundus mucosal ablation (GFMA). The procedure ablates the cells in the gastric fundus, the main site of the hunger-inducing hormone ghrelin. Patients also received nutritional counseling to promote healthy food choices.
Dr. McGowan had hoped that disrupting ghrelin production would reduce hunger and promote weight loss but was unsure how the body would adapt. “When someone loses weight, the body adjusts and progressively increases ghrelin in an attempt to stabilize weight,” says Dr. McGowan. “Obesity and weight are very complex. They’re regulated by multiple, redundant hormone pathways designed to maintain weight.”
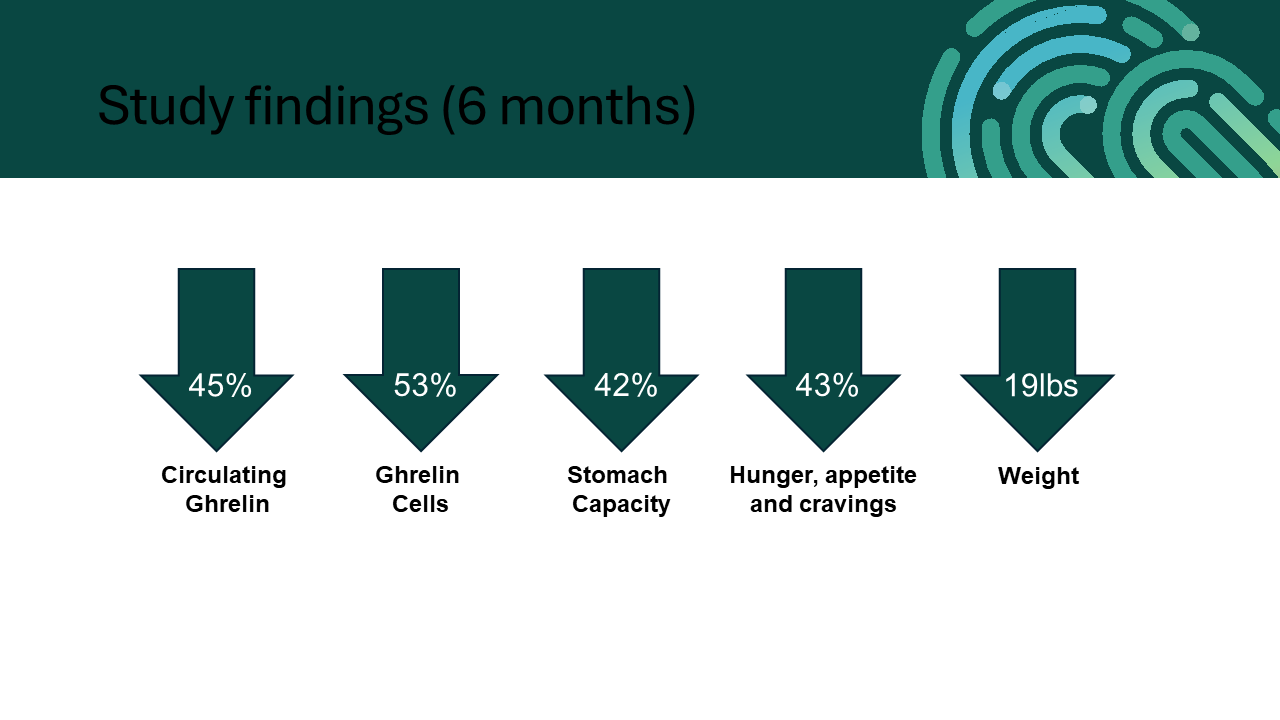
Key findings at six months following the procedure include:
- Patients lost approximately 8% of their body weight, an average of 9 kg.
- Plasma ghrelin levels decreased by 48% from 462 pg/mL to 255 pg/mL.
- Gastric capacity decreased by 42% from 807 mL to 467 mL.
- Histologic assessment showed a 54% reduction in ghrelin-producing cells by immunohistochemistry .
- Patient-reported hunger and Eating Drivers Index decreased significantly.
- Patient-reported control over eating, as measured by the Weight Efficacy Lifestyle Questionnaire Short-Form, increased significantly.
- The procedure was safe, with no serious adverse events.
Currently, the only way to significantly reduce ghrelin levels is to remove or bypass part of the stomach, as in weight-loss procedures such as the surgical sleeve gastrectomy. According to Dr. McGowan, this is the first study to reduce ghrelin via endoscopy in humans.
The study shows a promising impact on weight and serves as proof-of-concept for gastric mucosal ablation. Further studies are needed to assess the long-term outcomes of these techniques and whether the ablation of a larger territory beyond the fundus may have an even greater impact.
Dr. McGowan notes that it remains to be seen how GFMA may fit into the management of patients with obesity. Fundus ablation may find a role as a standalone procedure for select patients, as an adjunct procedure to other weight-loss strategies, e.g., for those transitioning off weight-loss medications, or in combination with restrictive weight-loss procedures like the endoscopic sleeve gastroplasty.
“The reduction in gastric capacity and hunger is very attractive for patients,” he says. “Patients with obesity often speak about ‘food noise,’ persistent thoughts of eating and a lack of control. If we can address this by impacting the major hormone responsible for hunger, we may be able to give patients more control over their eating habits and ultimately help them improve their health.”
Dr. McGowan’s oral presentation, “Endoscopic ablation of the gastric fundus in adults with obesity: A first in human study” on Sunday, May 19, at 2:32 p.m. EDT is part of the session “The Current Insights in Bariatric Endoscopy.”



2 Responses
I will be there
See you there Scott!