
The evaluation and treatment of hepatitis C virus (HCV) has undergone dramatic changes in recent years, which practitioners need to be aware of, according to Richard K. Sterling, MD, MSc, FACP, FACG, AGAF, FAASLD, professor of medicine and chief of the section of hepatology at Virginia Commonwealth University. He will outline the most recent developments and how gastroenterologists can adapt them in a presentation at Digestive Disease Week® (DDW) 2022.
“In general, HCV evaluation and testing has become much simpler,” said Dr. Sterling. “Gone are the need for liver biopsy and the side effects of interferon-based therapy. Assessing liver disease severity can now be done with a simple blood test, and direct-acting antiviral regimens are very well tolerated and highly effective.”
Sterling stressed several key points:
Everyone should be tested at least once.
New recommendations by the United States Preventive Services Task Force (USPTF) advise that everyone between the ages of 18 and 79 get a one-time screening test for HCV. Adults with ongoing behavioral risk factors such as illicit drug use, high-risk sexual behavior, or new diagnosis of HIV or HBV may be tested more often.
“Initial screening is often done by primary care, but it doesn’t have to be,” said Dr. Sterling “We as a GI community have an opportunity to make sure that HCV screening doesn’t fall through the cracks.”
Assessing disease severity is simple and noninvasive.
In patients with confirmed HCV viremia, simple, non-invasive tests are available to assess disease severity (fibrosis). Dr. Sterling highlighted the FIB-4 index, a blood-based test, as well as imaging-based tests that measure liver stiffness.
“If I have the blood test and the liver stiffness measurement, I can tell very well if a patient does not have advanced fibrosis and with moderate certainty if they do,” said Dr. Sterling. “That’s all I need to get them on treatment.”
Out of 10 FDA-approved direct-acting antiviral regimens, two have risen to the top for first-line HCV treatment. These regimens, consisting of all-oral, once-daily DAA therapy for 8-12 weeks, achieve excellent sustained virologic response (SVR) and are very well tolerated. Factors like HCV genotype, HIV coinfection, compensated cirrhosis and renal failure, which once warranted different treatment approaches, no longer impact HCV treatment choices. More complex patients, such as those with decompensated disease and those who fail DAA treatment may still need to be seen by a specialist.
“GI doctors can do all the first-line treatments and leave the more complex patients and failures to the specialists,” said Dr. Sterling.
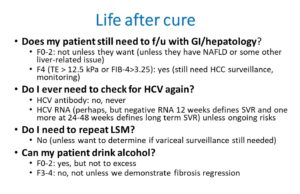
Physicians now need to consider life after cure.
With most treated patients being cured, life after cure has become an important issue. Topics to consider include determining who needs to continued follow-up for hepatocellular carcinoma (HCC) or variceal surveillance. In addition, many may need continued counseling and follow-up for behavioral and lifestyle factors, such as alcohol use and management of coexisting fatty liver disease.
Challenging patient populations remain.
Dr. Sterling described the need for strategies to increase patient compliance and to find effective treatment options for those with hepatic decompensation or significant comorbidities, such as advanced HCC.
Dr. Sterling will give the oral presentation, “Hepatitis C in 2022: What you need to know” on Monday, May 23, at 8:20 a.m. PDT as part of the symposium “Hepatology for Gastroenterologists.”



2 Responses
What lifestyle measures we should advise HCV infected patients?. Any family screening needed?
It is very good information about some myths regarding the curing of both HIV and hepatitis C infection. It was somewhat useful for many including me. It is a must-read blog to explore the new info about HIV and hepatitis C infection curable medicines . Keep it posting these kinds of informative blogs in the future!