New evidence is changing the management of alcohol-associated liver disease (ALD) — and hepatologists must be at the forefront, according to Brian P. Lee, MD, MAS, assistant professor of clinical medicine at the University of Southern California. Dr. Lee is presenting on the topic at Digestive Disease Week® (DDW) 2023.
“ALD-related mortality is at a historic high,” said Dr. Lee. “It’s time for hepatologists to step up and do more than treat the complications of liver disease. We need to address upstream factors, such as managing alcohol use disorder and addiction.”
Dr. Lee outlines several evidence-based approaches to reduce the impact of ALD.
Public policy can significantly impact alcohol use and related outcomes.
A recent study in The Lancet presented the impact of a 2018 law in Scotland that set a minimum price per unit of alcohol. The three-year results showed the following:
- Alcohol sales decreased by 3%.
- Alcohol-related hospitalizations decreased by 4%.
- Alcohol-related deaths decreased by 13%.
- The strongest impact was seen in socioeconomically deprived areas.
“The highest public health burden from alcohol is due to the heaviest users, who often opt for the cheapest alcohol,” said Dr. Lee. “This study showed that targeted, evidence-based government intervention can reduce alcohol-related mortality and disparities.”
Hepatologists must present a consistent, updated message on alcohol use.
“New research data has shown that there is no safe level of alcohol use,” said Dr. Lee. “If doctors are telling patients that 1–2 glasses of wine per day may have health benefits, that’s false and based on outdated data. Patients deserve to base their decisions on correct information.”
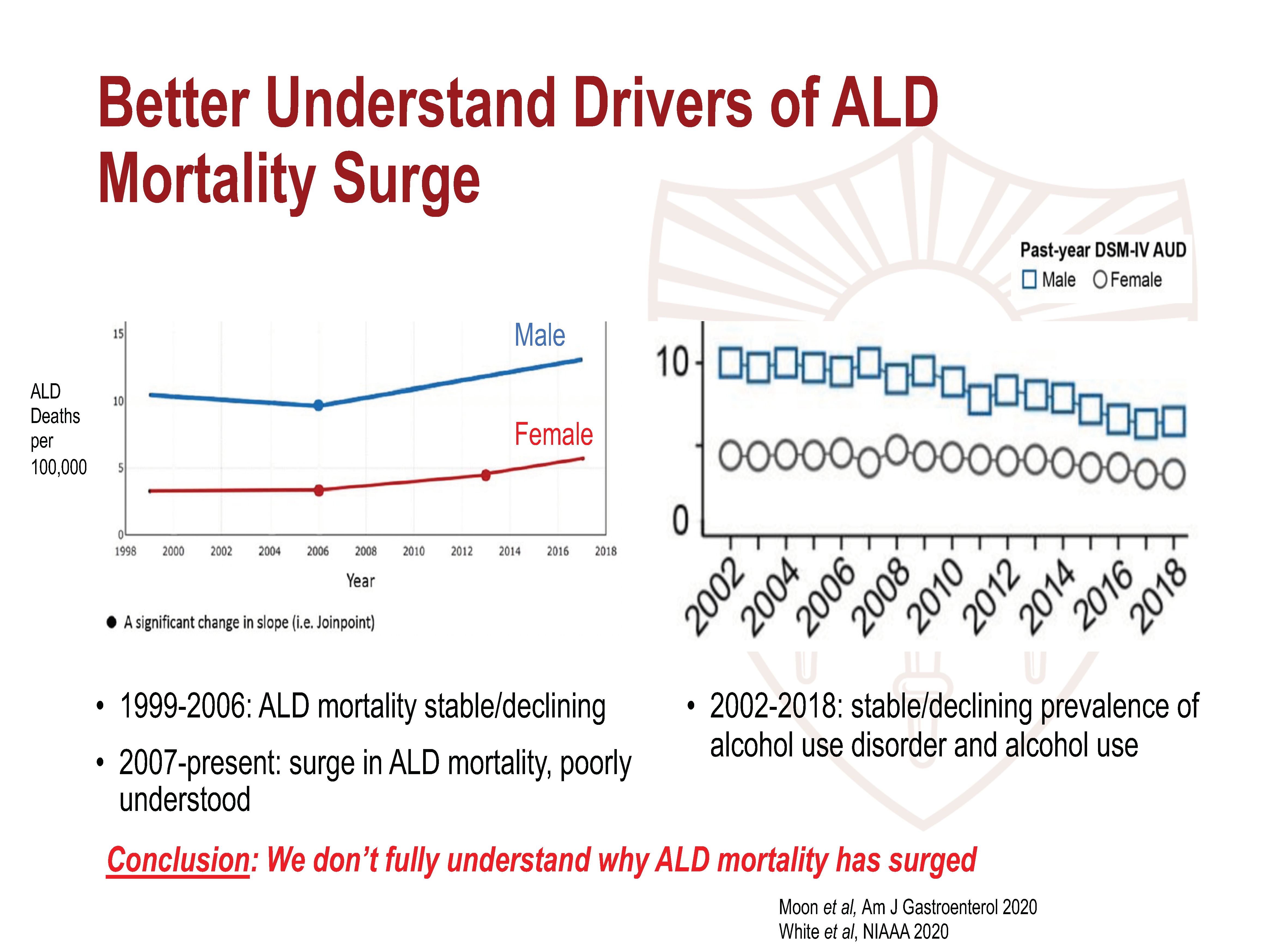
More research is needed to understand ALD-related mortality.
ALD-related mortality is at a historic high. However, except for a surge in alcohol consumption during the COVID-19 pandemic, the use of alcohol actually had been declining in recent years. Dr. Lee calls for more research to understand what drives alcohol-related mortality in the absence of increased consumption.
New evidence-based approaches for alcohol-associated hepatitis.
New criteria now makes it possible to diagnose alcohol-associated hepatitis based on clinical features and lab tests alone, without the need for a liver biopsy.
Dr. Lee is also optimistic that ongoing clinical trials may soon lead to effective therapies, but he stresses that the only intervention shown to promote positive long-term outcomes is treating alcohol use disorder.
Transplants for ALD no longer requires six months of sobriety.
Dr. Lee calls for a more comprehensive approach to selecting patients for transplant because emerging data has shown that six months of sobriety is not a reliable predictor of post-transplant alcohol recurrence.
“Requiring six months of sobriety was unfairly precluding transplant in patients who needed it,” said Dr. Lee. “We are now taking a more personalized approach that includes all risk and protective factors and is more founded on evidence.”
Hepatologists must be involved in managing alcohol use disorder.
Dr. Lee urges hepatologists to take on the responsibility of managing the upstream causes of ALD, namely alcohol use and addiction. But he said many practitioners do not feel prepared.
According to a recent AASLD survey of primarily hepatology and gastroenterology providers:
- 71% have never prescribed medications for alcohol use disorder.
- 77% reported low addiction training.
- 90% desired more formal GI/hepatology training.
Hepatologists need more education and resources to empower them to treat alcohol use disorder, Dr. Lee stresses. He described tools implemented at his hepatology clinic, including a standardized motivational interviewing approach and a flowchart to prescribe pharmacotherapy.
“The vast majority of hepatologists do not feel they have enough training in treating alcohol use disorder,” said Dr. Lee. “There’s also a perception that they don’t have enough time. We’ve shown that relatively simple interventions can be incorporated into a busy hepatology clinic and have a significant impact on patients.”
Dr. Lee’s lecture, “Controversies and consensus in alcohol-associated liver disease: past, present future” on Tuesday, May 9, at 10 a.m. CDT, is part of the session “AASLD Alcohol Associated Liver Disease: Controversies and Consensus.”