
Transplant centers might want to reconsider immediately rejecting a patient based on traditional criteria for liver cancer. Recent studies show that carefully selected patients with historically untransplantable liver cancers can not only be successfully transplanted but can also achieve good long-term outcomes, according to Anjana Pillai, MD, associate professor of medicine at The University of Chicago, who spoke on the topic at Digestive Disease Week® (DDW) 2022.
“Transplant centers must decide whether they are willing to take the risk of offering a liver transplant to patients beyond the Milan and UCSF criteria,” said Dr. Pillai, “Recent data have shown that you can push the boundaries, but careful patient selection and follow-up are critical.”
Transplanting beyond the Milan criteria in HCC
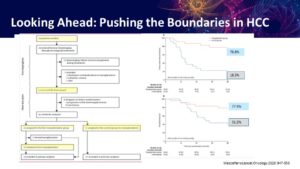
For hepatocellular carcinoma (HCC), the Milan criteria outline disease features that would make a patient an acceptable candidate for liver transplant. Immediate disqualifiers include high tumor burden, metastasis and vasculature invasion. However recent studies have pushed beyond the Milan criteria. Dr. Pillai showed data in two groups of patients — those with high tumor burden and those with side branch portal vein invasion — who were successfully transplanted following downstaging and who achieved long-term survival that surpasses what is typically achieved with current approaches.
“If your patient presents with multifocal liver cancer or vascular invasion, don’t automatically think they’re not a transplant candidate,” said Dr. Pillai. “Careful patient selection and stability are critical when you want to push beyond criteria. Look at the tumor biology. See if they could be downstaged to within the criteria. Once you downstage, wait six months to a year and reassess to see whether transplant is an option.”
Dr. Pillai stressed that these studies are small and that patients were carefully selected. All patients were successfully downstaged with locoregional therapy and/or chemotherapy and followed up for at least six months before being offered a transplant. Nonetheless, these data do suggest a broader approach to deciding who should be considered transplantable.
Dr. Pillai also presented data for transplanting patients with intrahepatic cholangiocarcinoma (bile duct cancer) and unresectable colorectal liver metastasis, which are currently considered untransplantable. Similar to the HCC studies, these studies were small, and patients were carefully selected.
“We are seeing a lot of younger patients presenting with advanced colon and bile duct cancer,” she said. “They generally don’t have a lot of risk factors. To be able to offer them a transplant and give them longevity beyond traditional chemotherapy is significant.”
“The decision of whether to transplant beyond current recommendations must be made as a transplant team,” she continued. “We have specific protocols at our center for these cancers, and we look at each case individually and carefully. The transplant team has to decide what they’re willing to accept with regard to recurrence and survival rates.”
Dr. Pillai will give the oral presentation, “Transplant oncology – advanced HCC and beyond” on Sunday, May 22, at 2:15 p.m. PDT as part of the session “The Latest and Greatest in Liver Transplantation.”


