
Measuring frailty offers a unique methodology for risk stratification models to predict post-surgical complications, according to Deborah Keller, MD, visiting assistant professor and surgical outcomes researcher at the University of California, Davis, who spoke on the topic during Digestive Disease Week® (DDW) 2022.
“We have tools and calculators that are associated with post-surgical outcomes,” said Dr. Keller. “But nothing is predictive for all patients and all surgery types.”
Dr. Keller outlined why frailty is an ideal target to predict the risk of post-surgical complications.
Frailty is objective, quantifiable and readily available.
Frailty is measured in multiple ways, which all encompass assessing grip strength, walking speed and muscle mass. Dr. Keller focused on the correlation between frailty and sarcopenia — the loss of muscle mass and function — which can be directly measured via a computed tomography (CT) scan.
“Using machine learning and artificial intelligence, we’ve shown that sarcopenia and CT scan measures are directly predictive of post-surgical outcomes,” said Dr. Keller. “This is information that every surgeon has at their fingertips as they prepare for surgery.”
Frailty is directly related to clinically meaningful outcomes.
Surgical complications directly impact many areas of patients’ lives and are costly to hospitals. Frailty has been associated with clinically meaningful changes in things that matter to patients, such as strength, ability to do daily tasks, and discharge from the hospital.
Frailty is generalizable. It has been shown to be predictive of surgical outcomes for multiple surgery types.
Regarding gastroenterology, frailty is the only marker that has been validated as predictive of post-surgical outcomes in transplant, upper gastrointestinal and lower gastrointestinal surgeries.
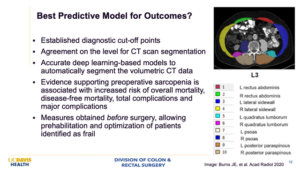
If a patient’s frailty score puts them at high risk for post-surgical complications, surgeons can work with patients to design a prehabilitation program to reduce their risk. Programs that combine strength, resistance and resiliency training along with information about surgery can help patients prepare for surgery and set them up for better outcomes
Dr. Keller stressed that the power of predictive markers such as frailty lies in facilitating discussions between surgeons and patients, empowering patients to confidently make an informed decision.
“There’s so much focus on enhancing recovery after surgery,” she said. “At that point, it’s too late. Go through the CT scans together with your patients and have conversations about their personal risk of complications and whether there are measures they can take to reduce that risk.”
Dr. Keller is working to develop point-of-care tools to make it easy and accessible to incorporate frailty into decision making and pre-surgery recommendations.
Dr. Keller gave the oral presentation, “Frailty: Better predictor of surgical outcomes?” on Sunday May 22, at 2 p.m. PDT as part of the “Frailty in Surgery” State-of-the-Art conference.


