Antibiotic use may be a risk factor for newly onset inflammatory bowel disease (IBD) among older adults, according to new data being presented at Digestive Disease Week® (DDW) 2022.
“We know that the incidence of IBD is rising in older adults, and we think that environmental factors are more important than genetics,” said Adam S. Faye, MD, MS, lead researcher on the study and assistant professor of medicine and population health at NYU Grossman School of Medicine. “When you look at younger patients with new diagnoses of Crohn’s disease and ulcerative colitis, there’s generally a strong family history. But in older adults, it seems that something in the environment is triggering it.”
Based on previous studies linking antibiotic use to onset of IBD in younger adults, Dr. Faye and colleagues at the Danish National Center of Excellence PREDICT Program and Mount Sinai examined whether this connection applied to older adults. They tracked antibiotic exposure among 2.3 million patients aged 60 and older in the Denmark national registry who had no previous IBD diagnosis.
Between 2000 and 2018, amassing more than 22 million person-years of follow-up, the study found 10,773 new cases of ulcerative colitis and 3,825 new cases of Crohn’s disease. To reduce potential confounding factors from antibiotic prescription for symptoms of undiagnosed IBD, the researchers did not include any antibiotic exposure in the year prior to IBD diagnosis in their analyses. Key findings include:
- Overall, antibiotic exposure was associated with an increased risk of IBD. Any antibiotic use was associated with an increased incidence rate ratio (IRR) for the development of IBD (IRR 1.65, 95% confidence interval [CI] 1.58-1.71).
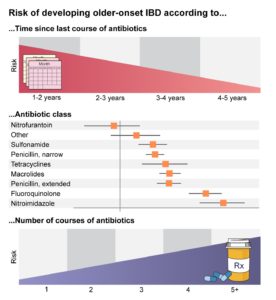
- A dose response was observed. The risk of developing IBD was higher in individuals who received more courses of antibiotics.
- The timing of antibiotic exposure mattered. The risk of developing IBD was higher in those who received antibiotics 1 to 2 years prior to their diagnosis but persisted even in those who received antibiotics 5 to 10 years prior to diagnosis.
- The type of antibiotic mattered. Most antibiotic classes were associated with an increased risk of IBD, except for those that do not impact the gastrointestinal microbiome, such as nitrofurantoin.
These data underscore the need for continued antibiotic stewardship and give clinicians more insight on when to suspect IBD in older patients.
“Diagnosing inflammatory bowel disease in older adults can be difficult because there is a broad differential,” said Dr. Faye. “If you know that patients have taken courses of antibiotics recently, perhaps IBD moves a bit higher on your differential.”
Dr. Faye cautioned that these data do not exclude the possibility that the underlying infections that prompt antibiotic use may be contributing to IBD, as opposed to the antibiotic itself. Future microbiome studies could help to distinguish these two potential triggers.
“These data support the idea that perhaps antibiotics are doing something to the gastrointestinal microbiome,” said Dr. Faye. “Even antibiotics that aren’t used to treat gastrointestinal pathogens but still impact the microbiome have a risk.”
Dr. Faye will present data from the study, “Antibiotics as a risk factor for older onset IBD: Population-based cohort study,” abstract 400, on Sunday, May 22, at 10 a.m. PDT.