
Understanding how to accurately identify most common liver lesions, knowing how to manage them and appropriately engaging in referral are crucial steps to ensuring correct diagnosis and avoiding delays in treatment, according to Barbara Andrews, NP, of the University of California San Diego Health System.
“It is important to focus on this topic because of broad differential diagnosis that can be associated with liver lesions,” said Andrews. “These lesions are often found incidentally when patients present to an emergency room for other medical issues. In addition to liver lesions, cirrhosis is often identified.”
Andrews presented case examples and imaging data to illustrate challenges in differentiating among the three most common types of benign liver lesions: hepatic hemangioma, focal nodal hyperplasia (FNH) and hepatocellular adenomas (HCA).
For example:
- In hemangioma, clinical presentations can be variable and many patients are asymptomatic. Imaging can help confirm diagnosis and should be repeated in patients with tumor >5 cm and a history of liver disease.
- For FNH, imaging with ultrasound is less useful for definitive diagnosis, as its appearance can mirror that of other types of benign lesions and even malignant lesions.
- “HCA is very challenging to diagnose, and that is where you really need to know your patient history,” Andrews said. “Are they cirrhotic? Do they have other liver disease? Do they have other cancers? Because in the setting of cirrhosis, a hepatocellular adenoma with this imaging is classic for hepatocellular carcinoma. And in other ways, it has that central scarring that can actually mimic an FNH.”
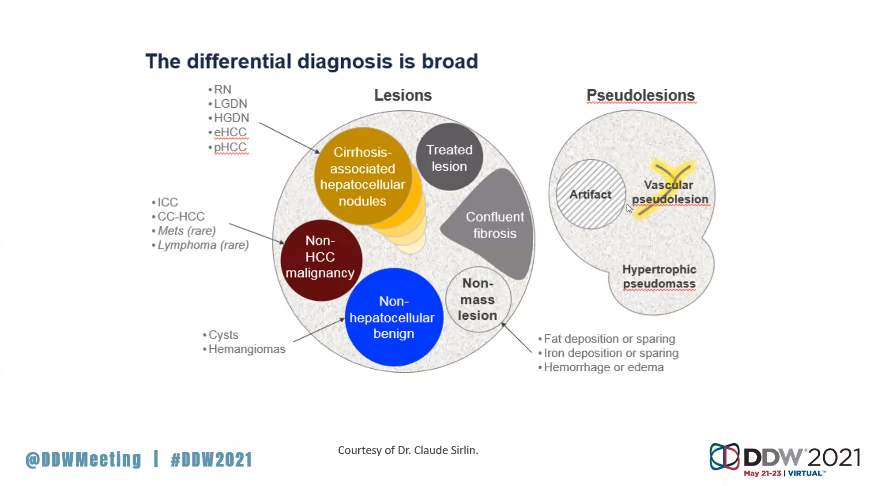
Diagnosis of malignant tumors — particularly hepatocellular carcinoma (HCC), which Andrews said accounts for about 85% of all primary tumors — can often be performed through imaging and without biopsy. In 2018, AASLD endorsed the use of the Liver Imaging Reporting and Data System (LI-RADS) for the surveillance and diagnosis of HCC.
“Utilizing the LI-RADS in patients at high risk for HCC provides a consistent framework to observe, describe and diagnose liver observations to guide surveillance and treatment options,” explained Andrews. “Referral to a hepatology specialist for further testing labs, clinical assessment and possible additional imaging will identify patients who need routine follow up for chronic liver disease. Early identification of liver lesions and chronic liver disease not only helps to direct the patient’s plan of care, it may also slow the progression of disease, fibrosis and/or improve cirrhosis.” Andrews’s oral presentation of “Liver Lesions 101” took place on Friday, May 21, at 1 p.m. EDT, as part of the AASLD session “Hepatology 101 for Associates: Abnormal LFTs, Management of Portal Hypertension and Liver Lesions.”



