
New practice guidance from the American Association for the Study of Liver Diseases (AASLD) addresses palliative care and symptom management for patients with decompensated cirrhosis. Shari Rogal, MD, MPH, assistant professor of medicine and surgery at the University of Pittsburgh and lead author on the AASLD document, discussed what hepatologists need to know about palliative care at Digestive Disease Week® (DDW) 2022.
“Palliative care is generally an underrecognized part of liver care,” said Dr. Rogal. “But it is critical to evaluate and address the palliative care needs of our patients with decompensated cirrhosis. While we have providers dedicated to palliative care, it’s important that patients know that they can talk about this with their hepatologist as well.”
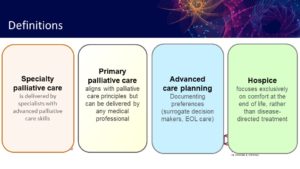
Palliative care encompasses a range of topics, but at its core it can be defined as patient-centered, symptom-focused care. The guidance document provides recommendations on many aspects of palliative care, including symptom management, supporting caregivers, advance care planning and end-of-life decisions. Dr. Rogal highlighted aspects of palliative care that are particularly relevant for hepatologists.
You can treat the underlying liver disease while providing palliative care.
Providers, patients and caregivers may have a misperception that palliative care is synonymous with hospice — focusing exclusively on patient comfort at the end of life. However, Dr. Rogal stressed that hospice is only a small part of palliative care. In fact, palliative care does not preclude transplant evaluation or disease-directed therapy and is appropriate to discuss with every patient with decompensated cirrhosis.
Dr. Rogal recommended that hepatologists bring up palliative care early in their conversations with patients and return to the discussion regularly as the patient’s condition, goals and priorities change.
“This is an ongoing conversation,” said Dr. Rogal. “A good lead-in can be something like “People with cirrhosis often have a lot of symptoms or aspects of their personal lives that impact their health. I want to make sure that we’re taking care of you the best way possible. What are some things that are important to you that we might not have talked about yet?’”
Prioritize and adapt your conversations as priorities change.
There can be a big disconnect between what is most important for patients and for physicians. Dr. Rogal recommended asking one or two probing questions during a visit to understand which symptoms are most important and to get a bigger picture of a patient’s mental health, social support system and values.
“Time is always a challenge,” said Dr. Rogal. “You have to prioritize what you talk about, and conversations will evolve as patients progress or their priorities change. These issues can be really nuanced, requiring shared decision-making with patients and caregivers.”
For example, pain management may require an ever-evolving discussion. “We spend a lot of time saying how bad opioids and benzodiazepines are for people with chronic liver disease,” said Dr. Rogal, “But at the very end of life, priorities change to focus on comfort. It can be hard to know when that point is for each patient, so open conversations with patients and caregivers about prognosis and values are critical.”
Palliative care is multidisciplinary, but hepatologists can play a critical role.
Palliative care is inherently team-based and multidisciplinary. Hepatologists should be aware of the resources at their site, such as social workers, psychologists, chaplaincy services and palliative care specialists. However, Dr. Rogal stressed that all providers can provide basic components of patient-centered palliative care. For example, it is never too early to assign a surrogate decision-maker in case the patient is unable to make medical decisions on their own.
Dr. Rogal gave the oral presentation, “Palliative care and end-stage liver disease,” on Monday, May 23, at 5:05 p.m. PDT as part of the “AASLD Practice Guidelines” workshop.



