The focus of attention for Barrett’s esophagus has shifted from finding treatments to finding patients, according to Srinadh Komanduri, MD, MS, associate chief of the division of gastroenterology and hepatology at Northwestern University. Dr. Komanduri participated in a case-based discussion on Barrett’s esophagus during Digestive Disease Week® (DDW) 2023.
“We have highly effective treatments for Barrett’s esophagus,” Dr. Komanduri said. “Cure rates are more than 95%. But we can’t find patients. The rising prevalence of esophageal cancer and new innovations for detection have us rethinking screening and surveillance so that more patients can receive effective therapy.”
New approaches to screening focus on asymptomatic patients.
Historically, screening for Barrett’s esophagus focused on a single risk factor—chronic gastroesophageal reflux disease (GERD). However, Dr. Komanduri points out that most patients with Barrett’s esophagus never develop symptoms and that risk factors such as smoking, obesity and family history have a higher predictive value than GERD.
A recent AGA Clinical Practice Update, which Dr. Komanduri helped develop, recommends that screening for Barrett’s esophagus be considered in individuals with three or more established risk factors. “For the first time, we’re opening the door to screening patients beyond heartburn-type symptoms,” Dr. Komanduri said. “We need to start looking at asymptomatic patients with risk factors.”
Less-invasive tools make broadening the screening population more feasible.
Dr. Komanduri notes that increasing the use of standard sedated endoscopies on asymptomatic individuals is not logistically feasible. Fortunately, new noninvasive screening tools, including non-endoscopic capsule-based methods and transnasal endoscopy, are more cost effective and less burdensome.
“We’re starting to see significantly less-expensive tools that could be applied to a larger population,” said Dr. Komanduri. “As gastroenterologists, we are already overstretched. These screening methods also have the potential to be done by advanced practice practitioners and technicians for scalability.”
Dr. Komanduri is testing ways to operationalize the use of these screening tools. For example, high-risk patients coming in for routine colonoscopy could be flagged in the electronic health records and undergo screening for Barrett’s esophagus during the same visit.
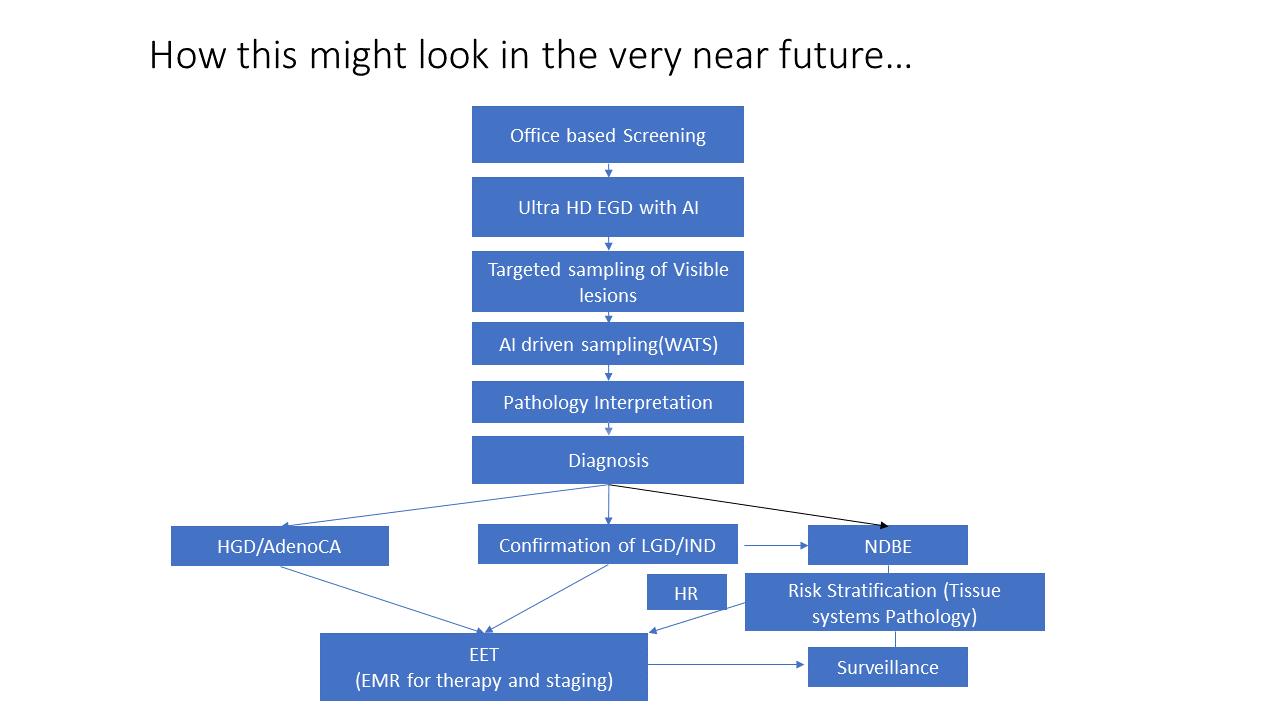
High-quality exams and innovations in artificial intelligence (AI) aim to reduce the incidence of post-endoscopy esophageal cancer.
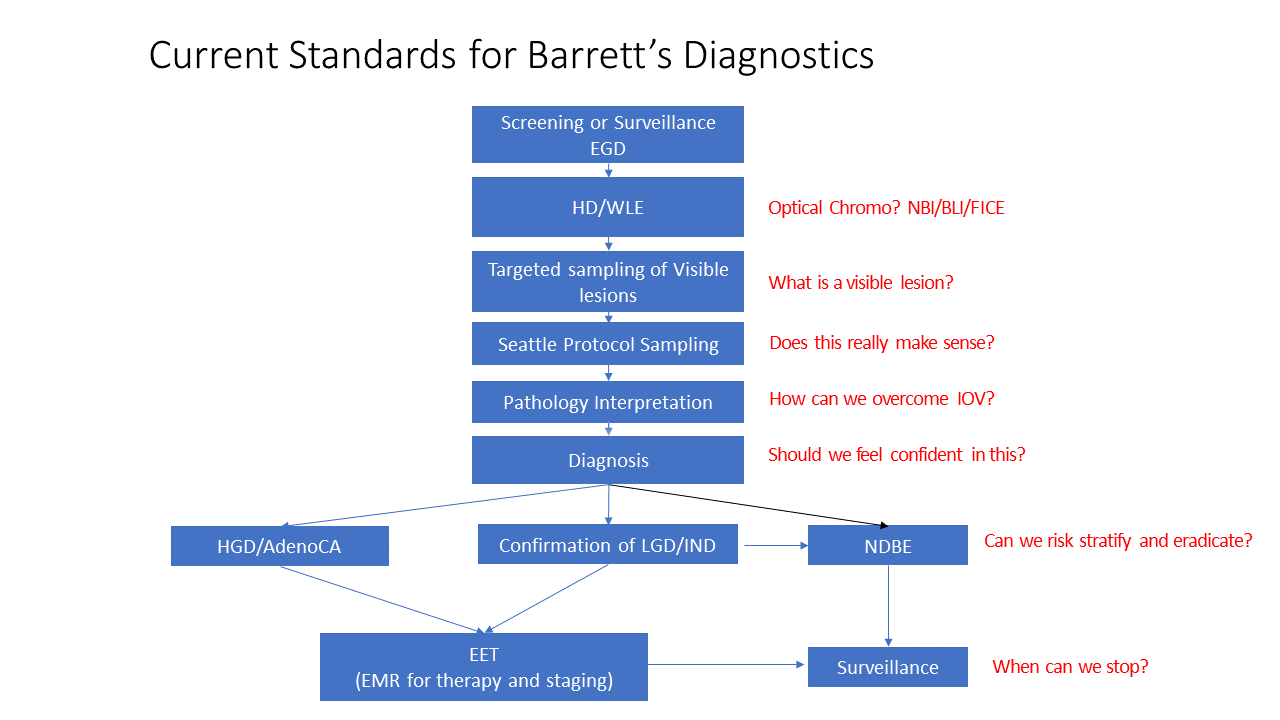
Multiple studies have shown that the rate of missed dysplasia among patients with Barrett’s esophagus is approximately 13%. Improving the quality of surveillance endoscopies is therefore imperative to reduce the incidence of esophageal cancer, Dr. Komanduri stresses.
Experts have agreed upon quality metrics and best practices for a high-quality exam. But often, these are often not documented or done well. He highlighted three recent innovations that may improve monitoring.
- AI algorithms are being developed to better identify lesions and may be useful in physician training.
- Wide-area transepithelial sampling can increase the yield of dysplasia detections and is currently being evaluated as an adjunct in high-risk patients.
- TissueCypher® provides a 5-year risk prediction score for esophageal cancer based on tissue analysis of known mutations.
“In terms of monitoring, the focus is on going back to basics,” said Dr. Komanduri. “The contractility of the esophagus makes it very challenging to find lesions. We need better training to conduct high-quality exams. At the same time, advances in AI may reduce the impact of human error.”
Mitigating recurrence after endoscopic treatment may reduce the need for long-term surveillance.
Dr. Komanduri said that increased attention is being focused on the minority of patients with esophageal cancer who recur. Uncontrolled reflux has been identified as a key risk factor for recurrence and may warrant anti-reflux procedures.
He is hopeful that many patients may not need continued surveillance. “Disease recurrence plateaus after 2–3 years,” he said. “If a patient makes it beyond that, they almost never recur. We are almost at a point where we may not need post-treatment surveillance.”
Dr. Komanduri participated in a case-based discussion on Barrett’s esophagus on Sunday, May 7, at 10 a.m. CDT as part of the session “ASGE Endoscopic Challenges in Barrett’s Esophagus.”
If you’re attending DDW, your registration includes access to a recording of this session, available to watch at your convenience until May 17, 2024. Session captures will be released 24 hours after the session ends. Non-attendees can also purchase access to DDW On Demand to watch session recordings after DDW ends.