As the only known endoscopic risk factor for esophageal adenocarcinoma, Barrett’s esophagus must be safely and effectively managed to help improve patient mortality. And recent innovations in cryotherapy and tissue resection are providing new help for patients with Barrett’s esophagus who might be at high risk for disease progression — particularly those who have previously failed standard therapy.
“There’s been a lot of advancements in devices in the past year, particularly in cryotherapy. This has been a big year for devices and ablation,” said Kenneth Wang, MD, of The Mayo Clinic, who presented on the topic at DDW® 2021. “And the second major area of advancement has been in endoscopic resections.”
Examples of new technologies include the following:
- In cryotherapy, a focal cryoballoon device is now available that allows the endoscopist to directly control the device (rather than an assistant doing so), includes foot pedals so the endoscopist can control the movement of the nozzle inside the esophagus, and features a user programmable jet of nitrous oxide that freezes the esophageal mucosa.
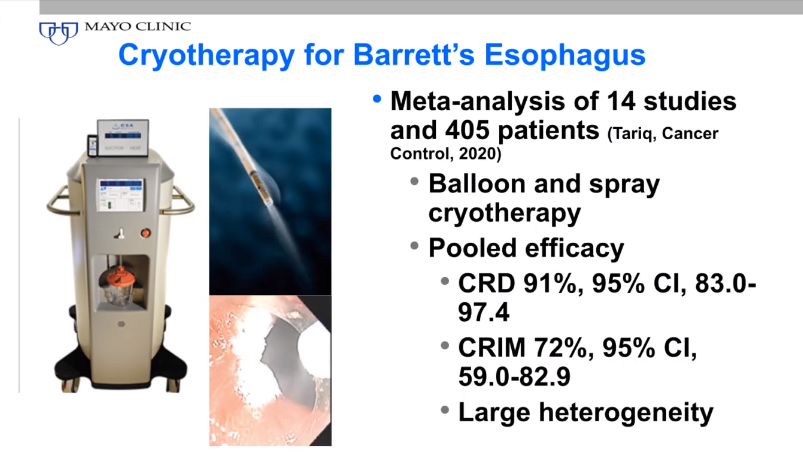
“There’s a fair amount of information coming out about the balloon spray and spray cryotherapy, such as a recent meta-analysis that showed very similar efficacy compared with radiofrequency ablation, although these were not head-to-head comparisons,” said Dr. Wang.
- Wang also described a hybrid argon plasma coagulation (APC) device that now has U.S. Food and Drug Administration approval, which combines APC with submucosal saline injection. The endoscopist injects fluid into the mucosa, which lifts the mucosa and creates a “cushion” wherein tissue can be ablated without doing any deep damage to the esophagus.
- In terms of resection devices, a novel articulating knife that operates more like scissors allows endoscopists to work more efficiently with reduced complications of endoscopic submucosal dissection.
- Finally, a new automated endoscopic resection device — originally developed for removal of adenomas in the colon — gives endoscopists more precise suction and deep tissue resection, but is non-thermal, meaning it carries an increased risk of bleeding.
Although these devices seem promising, Dr. Wang emphasized that radiofrequency ablation is still the first-line treatment, and that the hybrid APC or cryotherapy approaches should be considered once patients have failed radiofrequency ablation. Moreover, he emphasized that these novel ablation devices are most useful for persisting nondysplastic Barrett’s esophagus.
The resective techniques, on the other hand, will most benefit patients with persistent dysplastic Barrett’s esophagus — that is, patients considered more serious in terms of risk and progression, he said. But these too should only be used in cases of failure with first-line ablation therapy.
“These advancements give us more tools before the patient is referred to esophagectomy, which is recognized to be a major operation,” said Dr. Wang. “It’s good to have alternatives; that’s what this is all about. It’s good to have something else to offer, because that’s where the patient benefits, from avoiding a major operation, especially since patients with high-grade dysplasia in Barrett’s esophagus are older and have multiple co-morbidities.”
Dr. Wang’s oral presentation of “Updates in endoscopic treatment for Barrett’s esophagus” took place on Saturday, May 22, at 3:30 p.m. EDT, as part of the SSAT session “State-of-the-Art Conference: The Evolution of Endoscopic GI Surgery.”



