
Although pulmonary dysfunction is a highly common manifestation of symptomatic COVID-19 infection, hepatic injury can and does occur and may be particularly relevant in severe and long-term COVID-19 infection, according to emerging data from case reports, meta-analyses and retrospective cohort studies.
“We are not talking about liver abnormalities in patients with COVID. This is actually COVID-related liver disease,” explained Nancy Reau, MD, of Rush University Medical Center, who discussed this data during a presentation at DDW 2021. “Higher liver enzymes have a strong association with a bad prognosis, such as longer hospitalization and increased likelihood of death. But we are also starting to recognize actual liver complications related to COVID-19.”
Findings from a recent meta-analysis of liver manifestations and outcomes in COVID-19 confirm the heterogenous nature of the virus and variability in liver involvement before, during and after infection. Dr. Reau noted that this underscores the importance of large-scale, longitudinal data collection, such as that being undertaken by the National Institutes of Health, to better understand what happens to patients in the long run.
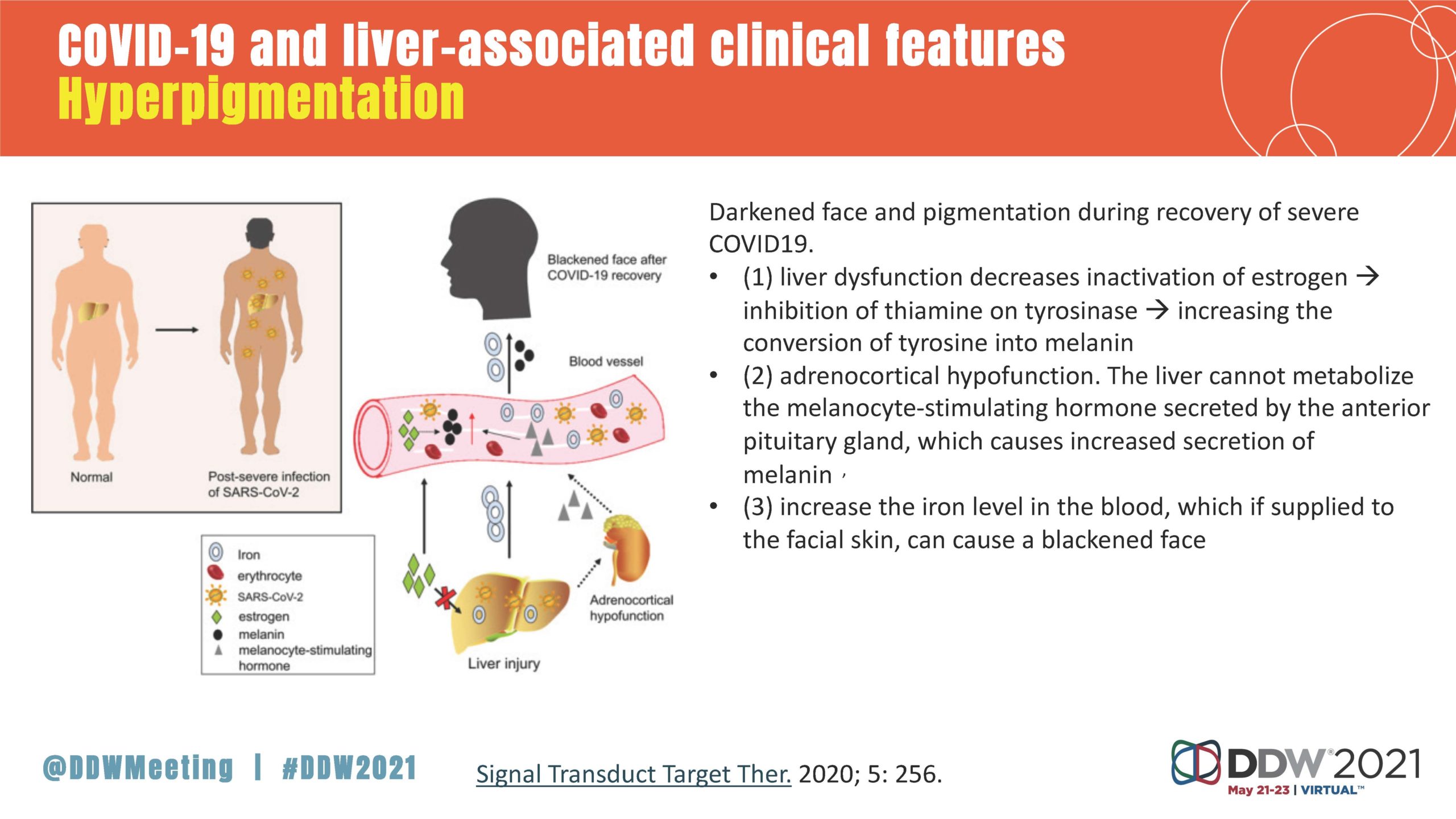
The potential pathophysiology of liver injury from COVID-19 is likely varied, including the direct targeting of hepatocytes by the virus, drug hepatoxicity, systemic inflammation and multiorgan damage, Dr. Reau said. Liver enzymes are often elevated in people hospitalized with the virus, but that cannot solely be used to determine the patient’s outcome, because these elevations are frequently mild and remit as COVID-19 improves.
“COVID-19 isn’t really a liver disease, but there are liver abnormalities in some people, although most are probably secondary,” Dr. Reau said. “If liver tests go up, that’s not necessarily COVID destroying the liver. You should always check for alternative explanations, like hepatitis B and C. And some people might be at risk for prolonged injury. So clinicians should not discount when a patient has recovered from COVID but may still have a liver problem.”
“The title of this talk is, ‘Hepatic manifestations of COVID-19: Is there cause for concern?’ And the answer is no; this is not a big area of concern for most people,” Dr. Reau said. “But some of the signals around this late cholestasis is the most important thing for clinicians to be aware of, because these are people who come in with a normal functioning liver and leave with it not as normal as it should be. So, how do we follow this? Are there going to be therapies? There’s really, unfortunately, a lot of unknowns about this infection.”
Dr. Reau’s oral presentation of “Hepatic manifestations of COVID-19: Is there cause for concern?” took place Sunday, May 23, at 1 p.m. EDT, as part of the AASLD session “COVID-19 and the Liver: Essential Updates for the GI and Hepatologist.”




One Response
How do we treat this condition ? Just observing ?